STROKE TIPS
Stroke Poem
Campaign for the Brain
By Jolene R. Marshall-MSN RN, SCRN
The human body’s most complex part,
To say a “Crown Jewel” is only a start.
This 3-pound organ in a bony shell
Protected by fluid, containing billions of cells.
It interprets senses, initiates movement,
Controls behavior; an intelligence unit.
It’s who one is, what’s said, what’s done
It defines humanity- all in one.
In a matter of seconds, minutes or hours
A clot can rush in and take all its powers.
A vessel may clog, take vision or speech,
Cause confusion, take senses, and even one’s reach.
Two million brain cells lost every minute
You won’t get them back so you’ve got to prevent it.
Be aware and competent; don’t miss the signs.
We can prevent disability and save more minds.
Save the Brain–Act FAST—Now!
A change can be missed; you need to know how.
Vital signs, Chemstick, Last known well
Call for help and Check “Neuro” to tell.
Are they moving all 4’s, awake and alert?
Vision, speech, a-fib to convert?
Be ready for any, for all, to save brain
Help scatter this message of the Brain Campaign
When suspicious of stroke, please dial 911.
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Interview on Doctor Radio’s Cardiology Show
Recently, I had the pleasure of participating in an interview on Doctor Radio’s Cardiology Show to discuss stroke preparedness. Please take a moment to listen in by following the link below.
https://mcspr.box.com/s/w23hwypw7nau6066lkzshgo43d7no9nh
When suspicious of stroke, please dial 911.
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
The F.A.S.T. Song
I hope you enjoy this very informative song about stroke prevention and awareness.
When suspicious of stroke, please dial 911.
Until next time,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
The Mobile Stroke Unit
A Mobile Stroke Unit (MSU) is an ambulance with a CT scanner installed and the personnel necessary to evaluate and treat a person with suspected stroke anywhere, anytime. The clot buster, tPA, can be given in the MSU prior to transport to a stroke center for monitoring, diagnostic studies, evaluations by therapists, etc. In addition to paramedics, that MSU needs a CT technician to perform the CT scan of the head, an ICU level nurse to administer the tPA, and access to a neurologist (either in the MSU or via telemedicine) to determine eligibility for tPA. The goal is for the MSU to beat a standard ambulance to the scene, rapidly triage and get appropriate patients treated with tPA.
In a recent trial of MSU in the Houston area (Bowry et al. Stroke 2015;46), the average time from MSU on scene to tPA administration was 25 minutes. Keeping in mind that the goal for hospital arrival to tPA administration is <60minutes, the average time saved with this approach was 35 minutes… or 70 MILLION brain cells. This is a priceless victory for any stroke patient. How much does a MSU cost? About $800,000. Currently, there are only 2 MSUs in the US – Houston and Cleveland. If you hear anything in the news about mobile stroke units…. pay attention. This may be the future of stroke treatment delivery!
When suspicious of stroke, please dial 911.
Until next time,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
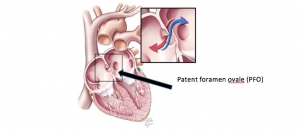
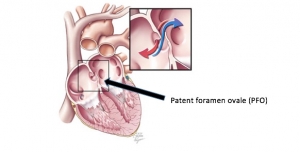
PFO and Stroke, Part II
So, a person has a stroke and a patent foramen ovale (PFO) is found on an echocardiogram or transcranial Doppler ultrasound. What should be expected? How does the finding of a PFO influence treatment? If the physician thinks the cause of the stroke could possibly be a clot which came from or across the PFO, evidence of more clot in the legs and/or pelvis is usually pursued with ultrasound and/or vessel imaging of the pelvis. If a clot is found, the treatment should be an anticoagulant (“blood thinner”) to treat the clot and prevent recurrent stroke and pulmonary embolism. If no clot is found, the treatment is usually an antiplatelet, such as aspirin. If the person was already taking aspirin, the physician may change antiplatelet medication, switch to an anticoagulant, or discuss closure of the PFO. With antiplatelet, the rate of stroke is about 1% per year.
Closure of PFO is possible during an angiogram. This involves accessing a large vein, usually in the groin, with a needle, advancing a closure device until it reaches the heart, crossing the PFO, and deploying the closure device. There have been three randomized clinical trials of PFO closure versus medical treatment (such as aspirin). The three trials had some differences in design and the patients who could be included and mixed results, but when the patients are combined and analyzed (meta-analysis), there is no protective benefit of closure versus medical therapy alone.
When suspicious of stroke, please dial 911.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
PFO and Stroke
Up to 25% of people have a Patent foramen oval (PFO) in their heart, however, less than 25% of people have a stroke. If you have a PFO, what does this mean for your risk of having a stroke?
We know that a higher proportion of patients with stroke have a PFO than patients without a stroke, suggesting that PFO may somehow be involved in the cause of stroke. Last week, we reviewed how a PFO may permit a blood clot to enter the brain circulation. But, if you follow a group of people with a PFO who have not had a stroke and compare their rate of stroke to that of a group of people who do not have a PFO and have not had a stroke, the rates are similar. This should mean that, if you have a PFO but no history of stroke, there is no reason for concern.
If you have a stroke, particularly if the stroke is classified as “cryptogenic”, there may be a greater chance of detecting a PFO than if another cause was identified. What is cryptogenic stroke? The word cryptogenic is derived from Greek and means “hidden cause.” Stroke is classified as cryptogenic when, after a reasonable work-up for the cause, the cause remains unknown. Work-up for a PFO is part of the evaluation of an otherwise cryptogenic stroke, particularly in patients < 50 years old, when other causes are less likely.
How is a PFO detected? There are three main tests used to detect a PFO: transthoracic echocardiography (TTE), transesophageal echocardiography (TEE), and transcranial Doppler ultrasound (TCD). In all cases, extremely small microbubbles are injected into a vein and evidence that the microbubbles cross into the arterial side of the heart from the venous side is sought. A TTE is an ultrasound of the heart performed by placing an ultrasound probe on the chest. This test is noninvasive and can visualize the microbubbles if they enter the left side (arterial side) of the heart. A TEE is an ultrasound of the heart performed by placing an ultrasound probe into the esophagus (swallowed by the patient). This test is invasive and requires sedation, but provides more detailed information about anatomy and is superior to the TTE in detecting a PFO. TCD is an ultrasound of the brain vessels and is performed by placing an ultrasound probe on the head, in regions with lower bone density. This test is inexpensive, noninvasive, does not require sedation, and has comparable ability to detect a PFO, but doesn’t provide information on the location of the “hole,” since it detects microbubbles which have entered the brain vessels.
Next week, I will cover the treatment for PFO after stroke.
When suspicious of stroke, please dial 911.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
What do you mean, “I have a hole in my heart?”
The human heart has 4 chambers: the right and left atria and the right and left ventricles. The atria receive blood and the ventricles push out blood. The right atrium receives blood from the body while the right ventricle sends blood to the lungs to get oxygen. The left atrium receives blood saturated with oxygen from the lungs, while left ventricle sends blood to the body. The atria are separated from the ventricles by valves. The right and left sides of the heart are separated by thin tissue called a septum.
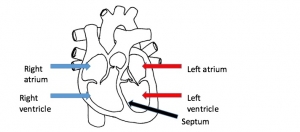
When there is a defect allowing blood to move between the atria, this is called an atrial septal defect. When there is a defect allowing blood to move between the ventricles, this is called a ventricular septal defect. Septal defects are one type of structural heart disease, a common cause of stroke in young children.
Before birth, it is normal to have an opening between the septum and the atria, the interatrial septum. Shortly after birth, the opening should close as the layers of tissue forming the septum fuse together. When this doesn’t happen, a person may have a patent foramen ovale.
Supposedly, 25% of us have this hole in our heart, a patent foramen ovale (PFO). How could this predispose to stroke? If a small clot forms in a vein where there is slow moving blood, it could travel to the heart. When this happens in someone without a PFO, it can go to the right atrium, then the right ventricle and then to the lungs. This is called pulmonary (lung) embolism (clot which traveled). It may cause no symptoms if the clot is very small, because the amount of lung injured is small. If the clot is large, it will block the blood flow to a larger part of the lungs and cause symptoms of chest pain and shortness of breath. Pulmonary embolism is sometimes fatal.
When a clot travels from a vein to the heart of a person with a PFO, the clot can cross from the right atrium to the left atrium and then to the left ventricle and then can be pushed out of the ventricle into the arterial blood supply. The clot could then travel to any part of the body, but will often, after being pushed up and out of the heart, continue traveling up towards the brain in the carotid or vertebral arteries. When this happens, blood flow to part of the brain is obstructed and a stroke can occur.
Next week, I will cover the work-up for a PFO. When is this important? What studies can be done to detect a PFO? The following week, I will cover the treatment for PFO after stroke.
When suspicious of stroke, please dial 911.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
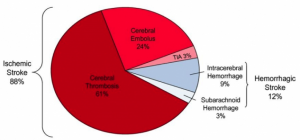
Stroke Facts
- Every 40 seconds, someone in our country has a stroke.
- 800,000 people in America have a stroke each year.
- Every 4 minutes, someone in our country dies from stroke.
- 130,000 people in America die from stroke each year.
- 1 out of every 20 deaths is due to stroke.
- Stroke is the #1 cause of long-term disability.
- Stroke is the #1 cause for new admission to a nursing home.
- Stroke costs the United states close to 50 billion dollars each year.
- Many of us have been personally affected by stroke through a family member or friend.
- Sadly, we Louisianians live in the Stroke Belt… the part of our country with the highest rates of stroke and stroke-related death.
- We have hope for better prevention, better treatment, and better recovery, but stroke awareness must be improved to achieve our goals.
- Please read through previous week’s posts to learn more about stroke.
When suspicious of stroke, please dial 911.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
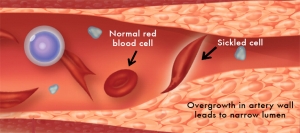
Sickle Cell Disease and Stroke
Stroke related to Sickle Cell Disease (SCD) can be prevented in most children by maintaining a low ratio of abnormal hemoglobin (hemoglobin S, as in Sickle) to normal hemoglobin (hemoglobin A). That target ratio is <30 abnormal hemoglobin out of every 100 red blood cells, or <30% abnormal hemoglobin (S). But how can the % of hemoglobin S be kept low?
The most effective way to keep the hemoglobin S within the target range is through exchange transfusion. Through a semi-permanent catheter (large tube placed inside a vein), blood is removed and usually replaced with normal red blood cells. Unfortunately, this catheter exposes children and adults to formation of blood clots, scarring of big veins, and infection, among other complications. Additionally, the exchange transfusion impacts quality of life due to the required frequency of treatment (several hours’ commitment for each treatment, as frequent as every 4 weeks). Regular exchange transfusion is not necessary or appropriate for all patients with SCD. Regular exchange transfusion has proven benefits to reduce stroke in persons with SCD and prior stroke and in patients with SCD without prior stroke, but with a high risk screening test.
Transcranial Doppler ultrasound (TCD) is the test used to distinguish patients without high risk for stroke. Transcranial means across the cranium or skull. Doppler ultrasound means that a pulse of energy is administered and information is received by the ultrasound machine providing information about the flow of blood through arteries of the brain. Narrowing of arteries leads to increases in the flow rate of blood. Only those patients determined to be at high risk for stroke based on TCD findings are referred for exchange transfusion. Patients who test at high risk and do not receive exchange transfusion have 10x the risk of stroke as a patient who tests at high risk and does receive exchange transfusion. This means that 90% of strokes in children with SCD can be prevented by exchange transfusion.
Stroke prevention begins, however, with detection of those children with SCD who are at high risk. Screening TCD is recommended for children with SCD annually from ages 2-16 when the prior study was normal and within 6 months for a borderline “conditional” or high risk test result. Once a high risk test has been confirmed with a repeat study, exchange transfusion should be pursued. Other treatments, including medication and bone marrow transplant are being examined, but nothing has been proven to be superior to exchange transfusion for prevention of stroke in children with SCD.
If you are the parent of a child with Sickle Cell Disease, know that your child should be screened with TCD each year to determine risk of stroke, exchange transfusion can drastically reduce the risk of stroke (if indicated by prior stroke or high risk TCD), and that children can experience stroke in subtle ways. In addition to sudden loss of vision, effective communication, strength on one side, sensation on one side, or clumsiness/incoordination, children may demonstrate seizure, sleepiness, reduced use of one side without complaining, headache, vomiting, or dizziness.
When suspicious of acute stroke, regardless of age, please dial 911.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Sickle Cell Disease and Stroke
First – what is Sickle Cell Disease?
Sickle Cell Disease (SCD) is a genetic disorder of hemoglobin primarily affecting African-Americans. One in every 400 African-American children have SCD. Hemoglobin is the primary substance of red blood cells and is responsible for carrying oxygen to our brain and body. Because having one abnormal copy of hemoglobin usually leads to no symptoms, the parents may be unaware that they have abnormal genes to contribute. When a child receives a specific abnormal copy of hemoglobin from both parents, the child can develop the disease. A child with sickle cell disease has two abnormal copies of hemoglobin, resulting in sickling (crescent shapes) of red blood cells. Sickled cells have harder edges than normal round red blood cells and do not move through blood vessels as well. The rough edges of sickled cells bounce into the walls of arteries, causing damage to the lining. Damaged arteries try to protect themselves by adding a layer of coating to the lining. Over time, this leads to narrowing of the lumen (opening) of arteries and increases the risk of stroke.
Children with SCD are at much greater risk of stroke than children without SCD. In fact, SCD is the most common cause of childhood stroke, affecting children between ages 3 and 14, leading to problems with learning, communicating, vision, walking, and/or performing activities of daily living. More than 15% of children with SCD have evidence of stroke on brain imaging, which are often “silent” (no obvious onset of loss of function).
There is a way to identify which children with SCD are at higher risk of stroke than others with SCD. There are treatments which can reduce the risk of stroke in children with SCD. Prevention is critical in high risk children with SCD. Next week, we will review these topics.
For any sudden severe headache with or without neck pain, or loss of vision, speech, strength, sensation, or coordination, call 911 to receive emergency treatment and limit disability.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
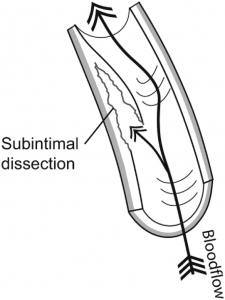
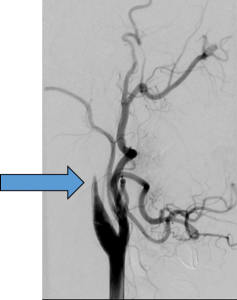
Dissection
Dissection is uncommon (<3 per 100,000 people), but is a relatively common cause of stroke in people <45 years old (about 15%). Dissection is the act of cutting something apart or separating one part of something from the rest. An artery is comprised of 3 major layers, the intima, media, and adventitia. When the intima is separated from the other layers, this is a dissection of the artery. When the artery is dissected, there may be pain along the course of the artery, loss of neurological function due to stroke, or sometimes no symptoms at all. The pain could be in the back or side of the neck and may radiate to the eye. Many people with a dissection have no complaint of pain. Many people who have dissection and pain in the neck have no stroke. This raises the possibility that many patients with dissection go without detection. Stroke can be caused by blockage of the normal artery by the tissue that was ripped away from the other layers or caused by a blood clot which formed on the downstream side of the torn artery. (See pictures below)
The separating of the layers of an artery is sometimes the result of trauma, including sports-related accidents, heavy lifting and abrupt movement of the neck (chiropractic manipulation, infection, coughing, sneezing, retching), and even sexual intercourse. Trauma can be minor and seemingly unimportant. Sometimes dissection is spontaneous. Neck pain preceding stroke symptoms increases the likelihood that a dissection will be found on blood vessel imaging (ultrasound, CT scan with contrast, MRI, or conventional angiogram). Arteries can also be dissected inside of the head. Similar pain can develop and so can stroke; however, dissection of arteries inside of the brain can cause bleeding in the fluids surrounding the brain, called subarachnoid hemorrhage.
Clinical studies of the best way to treat a dissection of an artery leading to the brain are limited. Many doctors will treat with blood thinners, such as heparin followed by warfarin. Others will treat with antiplatelet, such as aspirin. Sometimes, a procedure to stent the vessel open will be recommended. Treatment is individualized. Available data support the use of the clot buster, tPA, when a patient presents to the hospital with stroke symptoms present for less than 4.5 hours.
For any sudden severe headache with or without neck pain, or loss of vision, speech, strength, sensation, or coordination, call 911 to receive emergency treatment and limit disability.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Silent Strokes
What if you get a CT scan or MRI of your brain, for some other reason, and your doctor tells you that he or she can see that you had a stroke at some time in your life?
About ½ of all strokes are either clinically silent or were simply not detected by a physician. About 1 in 10 adults of advanced age have one or more strokes found on imaging, when there was no obvious stroke symptoms. Scary, right?
To be told that you have had a stroke, when you didn’t expect to hear this is scary, right?
The best way to live life without being scared of stroke is to live your life preventing and being prepared for stroke. If you or your loved one is told that a stroke was found on a CT scan or MRI of the brain, please schedule an appointment with your primary care provider or a stroke-treating neurologist to screen for a cause and optimize the medical therapy of all modifiable risk factors. Often, in the setting of evaluation of a new stroke, physicians discover conditions, such as diabetes or high cholesterol, which were unknown to the patient. These conditions represent targets for stroke risk reduction. Having had a stroke in the past is the most important risk factor for having another stroke. Usually, a medication such as aspirin is appropriate to prevent recurrent brain injury from stroke.
If you have had one or more silent strokes, you may notice some problems with thinking and memory that didn’t have a clear onset. These strokes matter and should be prevented once the risk has been identified.
For any sudden loss of function, call 911 to get immediate treatment and reduce long-term disability.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Cases of Vascular Dementia
There are 3 primary patterns of stroke and onset of vascular dementia.
- Multiple strokes without noticeable focal symptoms with slow, insidious, development of cognitive dysfunctionA 80 year old woman is brought in by her daughter due to concerns with memory and slowing of gait. The patient has had high blood pressure and diabetes for over 30 years. She has never experienced a stroke. She is found to have problems with concentration, short-term memory, and her arms and legs have trouble relaxing. The trouble with memory has been slowly progressive over the last 3-5 years. Her daughter is afraid to leave her home alone anymore, because she forgot the water running in the sink last week.
- Multiple strokes with noticeable focal symptoms with stepwise progressive development of cognitive dysfunction74 year old man with high blood pressure and who smoked until 2 years ago who has had 2 stroke in the last 6 years and other acute spells of unilateral weakness for which he refused to go to the hospital. His wife brings him to clinic with complaints of “not being able to take care of him since his last stroke.” With each of the strokes and more recent episodes of weakness, his ability to take care of himself, think of what he wants to say, and remember things has declined. He gets a little better between strokes, but never gets back to where he was functioning before each stroke.
- Single stroke in unlucky location with sudden development of cognitive dysfunction65 year old with high blood pressure who presented with complaints of headache. He was found to have problems with vision and with unawareness that he could not see on the left side. He was discharged home to his family. At follow-up, his family complained that he had poor memory, was losing important things such as his wallet or his keys, and became paranoid that his things were being stolen. He never recovered from these problems, requiring 24/7 supervision and medications to control his agitation.
There many faces of vascular dementia. The best way to treat it is to PREVENT it. Keep stroke risk factors under control. Seek immediate treatment for any new stroke symptoms/signs, to minimize disability.
Never forget… during a stroke, every minute counts. Dial 911 immediately if you experience any sudden loss of function – vision, speech, strength, coordination, sensation, balance, or a new severe headache.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Stroke Can Lead to Dementia
What is dementia? The word dementia is derived from Latin. De = out, ment = mind, ia = noun. So, strictly speaking, the word is defined as a state of being out of one’s mind.
We use the term dementia when a person has impaired memory and some combination of judgment, language/communication, and executive functions/complex tasks, such as paying bills or keeping appointments. The demented person may have psychological changes, such as inappropriate behavior, agitation, or paranoia.
Common causes of dementia include Alzheimer’s dementia and vascular dementia.
Vascular dementia is caused by progressive or recurrent damage to the brain resulting from impaired blood flow, often in tiny arteries. Unlike Alzheimer’s dementia, symptoms of dementia related to vascular dementia usually occur suddenly, in patients with pre-existing risk factors for stroke, like hypertension. Progression of vascular dementia tends to be stepwise progressive, meaning stable symptoms with sudden deteriorations, rather than continuously, but slowly progressive. The patient with vascular dementia generally has abnormal findings on neurological examination, such as unilateral weakness or numbness, and trouble with gait. Imaging (CT or MRI scan of the brain) can distinguish between vascular dementia and Alzheimer’s dementia.
Many of the small strokes leading to vascular dementia are subclinical and not detected by a physician. Subclinical means that the symptoms were very subtle or even un-noticed, and did not lead to evaluation and diagnosis of stroke. But these small strokes gradually contribute to loss of speed of information transfer and ultimately, dementia.
Next week, I will review a few cases of vascular dementia.
Never forget… during a stroke, every minute counts. Dial 911 immediately if you experience any sudden loss of function – vision, speech, strength, coordination, sensation, balance, or a new severe headache.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
FAST (part 2)
This is the abbreviated message about stroke symptoms and needed action.
F = face
A = arm
S = speech
T = time
Last week, we reviewed each component of FAST and learned that 89% of patients with stroke can be identified using FAST. This week, we will examine the symptoms and signs of stroke in the remaining 11% of patients with stroke.
Common symptoms and signs of stroke NOT captured by FAST include:
- Dizziness
- Change in or loss of vision
- Headache
- Confusion
- Leg weakness
Dizziness is a very nonspecific symptom if not characterized further. The potential causes of isolated dizziness or vertigo, an illusion of movement, often described as a spinning sensation, is fairly long and may include benign conditions, such as benign paroxysmal positional vertigo. Dizziness could be due to loss of blood flow to the pathways in the brainstem or cerebellum responsible for your awareness of position in space. Sudden dizziness or vertigo is usually associated with difficulty walking or loss of balance/coordination and is present in 44% of patients with stroke. In the absence of one or more of the FAST components (face, arm, and speech), 5.3% of patients with stroke will complain of dizziness.
Visual changes can include loss of vision in one eye, double vision, or loss of ability to see in one half or one quadrant of the visual fields. Sudden visual change or loss occurs in about 14% of all strokes. In the absence of one or more of the FAST components, 4.1% of patients with stroke will complain of visual symptoms.
Severe headache, unlike prior experienced headaches, particularly if associated by any other stroke symptom (weakness in any part of the body, trouble with speech or communication, loss of vision, etc) or associated with nausea or sleepiness could be due to stroke, and more likely due to hemorrhagic stroke. Sudden headache is present in 19% of all strokes, but 40% of hemorrhagic strokes. In the absence of one or more of the FAST components, 4% of patients with stroke will complain of headache.
Confusion is a nonspecific symptom, but can be due to sudden interruption of connections between brain regions involved in language, memory, or attention. In the absence of one or more of the FAST components, 3% of patients with stroke will have confusion present.
Leg weakness or numbness can accompany similar symptoms in the face and arm or could occur independently. In the absence of one or more of the FAST components, 1.7% of patient with stroke will have isolated leg weakness.
The FAST is effective in recognizing most patients experiencing stroke. If someone has sudden complaint of dizziness, visual change/loss, severe headache, confusion, or isolated leg weakness, he or she is probably having a stroke. Any sudden loss of function is a stroke until proven otherwise. Call 911.
Never forget… during a stroke, every minute counts. Dial 911 immediately if you experience any sudden loss of function – vision, speech, strength, coordination, sensation, balance, or a new severe headache.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
FAST (part 1)
FAST is a simple yet effective tool used to screen for stroke and to emphasize the time-sensitivity of responding (by dialing 911).
F = face
A = arm
S = speech
T = time
The face is affected by stroke in 39.1% of patients with stroke. Often, facial involvement is accompanied by slurred speech, called dysarthria. The facial weakness usually spares the forehead and is most noticeable during attempts to smile. The facial weakness is usually on the opposite side of the stroke; for instance, a right facial droop is usually due to a problem with the left side of the brain.
The arm is involved in stroke in 64.8% of patients with stroke. Often, the face and/or leg is affected on the same side of the body. There may be weakness, loss of sensation, or both. The weakness may be detected by having the person hold the arms out, perpendicular to the floor, for 10 seconds. If one side drifts down, there is weakness. There may be weakness not detectable by drift. Testing for grip strength may detect hand weakness without arm drift. The weakness may be detected by having the person hold the leg up, 30 degrees from the floor, for 5 seconds. If a leg drifts, there is weakness. Weakness and/or numbness is usually on the opposite side of the stroke.
Speech is affected in 56.5% of patients with stroke. Speech problems may be limited to trouble pronouncing words correctly, and may involve language problems such as expressing ideas, naming, reading, writing, repeating, or understanding. Speech can be quickly tested by asking a person to repeat simple words and phrases, name various items, or follow simple instructions (show me 2 fingers).
Time is critically important. Time to recognition, time to action (dialing 911), time to treatment. There are effective treatments to minimize or even reverse stroke symptoms, but with each passing minute, these treatments are less effective, because more brain cells have been permanently destroyed.
Next week we will cover the common symptoms and signs of stroke that FAST does not screen for. It is important not to miss an opportunity to respond FAST to a stroke when it occurs. Knowledge of common symptoms and signs of stroke and knowledge of the time-sensitivity of stroke treatments is crucial to reducing avoidable long-term disability and death.
Never forget… during a stroke, every minute counts. Dial 911 immediately if you experience any sudden loss of function – vision, speech, strength, coordination, sensation, balance, or a new severe headache.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Aspirin Use
Symptoms of a HEART ATTACK?
Chew an aspirin. Aspirin early after onset of heart ischemia is associated with improved outcome. There is almost zero chance your symptoms are due to a bleeding heart.
Symptoms of a BRAIN ATTACK?
DO NOT TAKE AN ASPIRIN. Aspirin in the first few hours has never been proven to influence the outcome. Depending on your risk factors, there is up to 20% chance that bleeding in the brain is the cause of stroke symptoms. Aspirin could be harmful to someone who is actively bleeding in the brain. Aspirin could make a hemorrhage get bigger by preventing the natural clotting.
Never forget… during a stroke, every minute counts. Dial 911 immediately if you experience any sudden loss of function – vision, speech, strength, coordination, sensation, balance, or a new severe headache.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
American Stroke Month
Please take this challenge….
This week , teach at least 5 people each day the following key facts:
- Stroke is a leading cause of death and the #1 cause of disability
- Stroke is preventable – the most important risk factor is hypertension
- Stroke presents with sudden loss of function – any function, but most commonly some combination of vision, speech, strength, coordination/balance, sensation or headache
- Stroke is treatable, but the treatment must be given FAST. With each minute after onset, the effectiveness of treatment is less.
- Stroke rehabilitation is essential for recovery of function. Improvements can be seen even years later with persistent effort.
Never forget… during a stroke, every minute counts. Dial 911 immediately if you experience any sudden loss of function – vision, speech, strength, coordination, sensation, balance, or a new severe headache.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Stroke Telemedicine pt. 3
How does telephone consultation compare to video-based telemedicine consultation for stroke?
The pros of telephone consultation include cost and speed of accessing expertise.
- A physician or other provider can pick up a phone, dial a number, and get access to a neurological expert within 60 seconds.
- There is no cost beyond the call itself.
- The information exchanged is based on a hypothetical patient.
- Unless the neurological expert has privileges at that hospital, he or she cannot review the brain images and makes a judgment call based on the information provided, including the interpretation of the brain images by another provider.
- Documentation is not necessarily performed.
- The neurological expert may be back to bed or business as usual in 10 minutes.
- There is no charge.
- There is limited liability.
- The patient and calling physician, or other provider, got what they needed…time sensitive advice
Video-based telemedicine consultation is more complicated to set up and costs someone something.
- Unless performed on a mission base, a hospital needing the access pays a fee to the hospital or organization providing the service.
Passage of information through technology requires compliance with standards for protection of patient data. - Troubleshooting connectivity requires access to an information technologist.
- Telemedicine can be rather simple, such as smart phone, tablet, or laptop/desktop two-way cameras.
- The neurological expert can interact with the staff in the hospital, the patient, and the patient’s family members.
- The expert can examine the patient, with some help from the hospital staff, review images, and discuss the care recommended with all parties.
- A consultation note can be documented, and, in some states, a charge for the service can be made.
So, how do these two methods for providing access to neurological expertise fair for acute stroke?
With telemedicine, one study found that the correct treatment decision is made more often than telephone consultation (98% vs 82%).1 For every 6 telemedicine consults, 1 more correct decision was made than if the 6 consults had been performed by telephone consultation. No differences in outcomes have been reported in a large sample of stroke patients.
1Meyer BC1, Raman R, Hemmen T, Obler R, Zivin JA, Rao R, Thomas RG, Lyden PD. Efficacy of site-independent telemedicine in the STRokE DOC trial: a randomised, blinded, prospective study. Lancet Neurol. 2008 Sep;7(9):787-95.
Telephone or video-based telemedicine consultations get the experts to the patients who need them, when they need them, regardless of the time of day or day of the week. Does your hospital have a neurological expert available?
Never forget… during a stroke, every minute counts. Dial 911 immediately if you experience any sudden loss of function – vision, speech, strength, coordination, sensation, balance, or a new severe headache.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Stroke Telemedicine pt. 2
Access to neurological expertise is associated with improved utilization of the clot buster, tPA. tPA doesn’t come without risk and the “rule book” is lengthy. If an emergency department physician has few exposures to patients with hyperacute stroke, experience is lacking and this may result in heightened anxiety when faced with a time-sensitive high-risk decision to make.
We’ve reviewed the time-sensitivity of treatment for stroke in several other tips. The risk is a real, though infrequent outcome of bleeding in the brain, making a person worse. This happens in less than 3% of patients who receive tPA; this means 97% of patients will not experience brain bleeding, worsening outcome. Keep in mind that tPA is the single medication proven to improve the chance of independence after stroke, by about 30% compared with outcomes of patients not given tPA. Therefore, the greatest risk to independence after onset of stroke is to allow the natural history and not stop the stroke from completing itself. But for that emergency department physician unfamiliar with the clinical trials and subsequent real-world experience with tPA for stroke, the fear of causing that infrequent brain bleed can be overwhelming.
When there is a large menu of hypothetical and real factors which increase risk, a decision to not treat may be less stressing than a decision to treat, particularly if access to an experienced neurologist is lacking. And believe me, access to experienced neurologists to guide treatment for stroke IS lacking, largely due to misdistribution of these specialists. It would take too long for many people to get to centers where stroke specialists are physically present, in many cases so long that the treatment would no longer be effective.
Because EVERY MINUTE MATTERS during stroke, the stroke specialist needs to get to the patient who needs him or her. One way to do this is to provide telephone consultation. With development of technology, stroke telemedicine was developed to fill the gaps in coverage and bring the neurologist to the patient. Stroke telemedicine involves the use of two-way cameras on computers, allowing the stroke specialist to interview and examine the patient, review brain imaging, and communicate with the emergency department physician and staff.
Next week, we will compare the pros and cons of telephone versus telemedicine for stroke.
Never forget… during a stroke, every minute counts. Dial 911 immediately if you experience any sudden loss of function – vision, speech, strength, coordination, sensation, balance, or a new severe headache.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Stroke Telemedicine pt. 1
I would like to share with you something that happened two days ago.
I was traveling by air to the mid-west to give an educational talk. I was seated next to an older couple traveling to visit their daughter. We started talking and when they learned about my occupation, they were clearly very interested. They sequentially asked all of the right questions. What causes stroke? What are the symptoms? Is there anything that can be done about it? I explained each of these things and discussed the time sensitivity of treatment for stroke.
As the conversation continued, they inquired which hospital in their area they should go to if either of them thought they were having a stroke. This was a particular interest to them because they live in a rural area. When we touched down, I looked up the closest certified stroke center (Primary Stroke Center) in their area by searching http://www.strokecenter.org/trials/centers/. It was about 150 miles away! I could tell they were concerned, so I explained the concept of stroke telemedicine and how I was able to handle stroke patients in rural areas through my fancy iPad. They fully intended to discuss this with their doctor and local hospital in order to determine if the necessary resources would be available to him or his wife, if ever needed.
Check back next week for more about stroke telemedicine.
Never forget… during a stroke, every minute counts. Dial 911 immediately if you experience any sudden loss of function – vision, speech, strength, coordination, sensation, balance, or a new severe headache.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Know Your Medications
Simple, yet important tip this week. Know your medications. Keep a list in your wallet, and keep that list up to date. During evaluation of a suspected stroke, physicians are considering whether you are eligible for the clot-buster, tPA. There are certain medications, “blood thinners,” which would theoretically increase the risk of serious bleeding and may be a reason why you would not be treated. Don’t make your doctor guess or lose time during your stroke to try to figure out what you are taking or when you last took your medication. Every minute matters when treating a stroke.
Your doctor will want to know if you are taking one of the following medications. Antiplatelets, such as aspirin, clopiogrel/Plavix, or Aggrenox are not reasons to withhold tPA, but warfarin/Coumadin with INR >1.7, injected heparin/heparinoids, and the new oral anticoagulant medications including:
- Dabigatran/Pradaxa
- Apixaban/Eliquis
- Rivaroxaban/Xarelto
A simple strategy would be to keep a medication list in your wallet and indicate “no blood thinner” or “no anticoagulant” if you are not taking one.
Never forget… during a stroke, every minute counts. Dial 911 immediately if you experience any sudden loss of function – vision, speech, strength, coordination, sensation, balance, or a new severe headache.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Reducing Stress
Last week, we covered a few of the conceptual ways that stress can lead to stroke. This week, we aim to provide some tips to reduce stress load.
The internet has over 27 million hits for the google search “tips to reduce stress”! What a popular topic!
Here is a summary of commonly cited tips.
- Keep a positive attitude. Try to see the bright side of a situation. Every challenge is an opportunity for someone to learn something new or develop a new skill.
- Avoid or limit time spent with people who consistently add to your stress, if possible.
- Set reasonable goals and expectations for yourself. This helps with time management. Learn how to say “no” if you recognize you are overstretched in commitments.
- Be clear about your expectations of others.
- If you feel tension/stress developing, take a break from the provoking factor, if at all possible.
- Take a few minutes each day for private time to relax. Consider meditation, focusing on positive thoughts such as “I can do this”, “I’m happy with my effort”, etc.
- Concentrate on breathing deeply for a 5 minute period of time with good posture and eyes closed. This has positive effects on heart rate and blood pressure.
- Exercise regularly.
- Avoid excess alcohol and recreational drugs – the aftermath never pays off and generally contributes to subsequent stress.
- Eat healthy and carry healthy snacks.
- Listen to music that is soothing or carries positive messages – or songs that get your body moving!
- Maximize your time for sleep and reduce disruptions. Before bedtime, consider investing in a neck pillow which can be heated and then applied to your neck and upper shoulders. But don’t oversleep.
- Access your support system regularly to maintain the connection. Being there for someone else will help ensure someone is there for you when you need it. Withdrawing from friends and family because you don’t want them to know you are having trouble or don’t want to bother them is contraproductive.
- Remember to be grateful for the family, friends, talents, knowledge, and health that you have.
- Accept that you cannot control every thing. Forgive yourself for your imperfections. Try to laugh at yourself for mistakes without serious consequences.
Never forget… during a stroke, every minute counts. Dial 911 immediately if you experience any sudden loss of function – vision, speech, strength, coordination, sensation, balance, or a new severe headache.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Acute Stress
I am often asked by patients….”Can stress cause a stroke?”
Acute stress is known to stimulate the sympathetic nervous system. This is your “fight or flight” system, during which adrenalin is released into the blood, pupils dilate, heart rate increases, and blood pressure increases. Sudden increase in blood pressure is the mechanism of many hemorrhagic strokes. The pressure on the wall of a small artery causes a tear in the wall, resulting in blood coming out of the artery and pooling inside the brain tissue.
Chronic stress can promote chronically elevated blood pressure, high blood sugar (diabetes), and is associated with poor choices – such as forgetting our medication, smoking, and drinking excess alcohol. High blood pressure, diabetes, smoking, excess alcohol, and not taking important preventative medications can increase the risk of stroke by promoting damage to the heart and arteries that supply blood flow to the brain. Chemicals released during stress may directly damage the heart and arteries as well. It is very difficult, if not impossible, for the impact of stress on stroke risk to be quantified, because there is no validated way to quantify an individual’s stress.
If you are struggling with stress, please talk to your doctor about this. Next week, we will cover tips to reduce stress.
Never forget… during a stroke, every minute counts. Dial 911 immediately if you experience any sudden loss of function – vision, speech, strength, coordination, sensation, balance, or a new severe headache.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
At the International Stroke Conference 2015, we learned about 4 clinical trials with encouraging results for endovascular therapy (see Stroke Tip of the Week February 16, 2015) for strokes caused by occlusion (blockage) of large brain arteries. At the end of the final presentation, it was declared that “Endovascular therapy for large artery stroke is standard-of-care.” This poses a major challenge for most of the world, since most hospitals cannot provide the expertise and specialized equipment to provide endovascular therapy. In Louisiana, a handful of hospitals can provide this therapy. How can we improve the access to this treatment?
Keeping in mind that most patients included in the positive trials of endovascular therapy FIRST received IV tPA, initial destination to hospitals that can safely and efficiently administer IV tPA (LERN Level I, II, or III hospitals) remains the best chance of recovery after onset of stroke. After evaluation and initial management, patients can be transferred to hospitals for adjuvant endovascular therapy (LERN Level I and some Level II hospitals), when appropriate. This does not mean that all patients need to be transferred to hospitals with endovascular capability. Patients with occlusion of large brain arteries represent a small proportion of stroke patients. In order to improve access to endovascular therapy for this small proportion of patients, hospitals need to be able to quickly identify which patients may benefit, identify the closest endovascular capable hospital immediately, and work as fast as possible to get patients transferred to these hospitals. A general rule is that it is faster to be transferred by air ambulance than ground if the distance is more than 45 miles between centers.
We can only expect improvement in outcomes similar to that detected in these trials if patients get the treatment as fast as it was provided in these trials.
For hospital staff:
To identify which patients may benefit from endovascular therapy, options include obtaining a CT angiogram at the initial hospital and transferring only those with large artery occlusions or using a stroke severity threshold, for example, the NIHSS score of at least 10 with at least 2 points from gaze, visual fields, aphasia, or neglect.
To identify the closest endovascular capable hospital immediately, the LERN Communication Center can be contacted readily at 1-866-320-8293.
Never forget… During a stroke, every minute counts. Working fast to get a potentially eligible patient transferred to endovascular capable hospital is just as urgent as the evaluation for and treatment with IV tPA. 2 million brain cells are dying with each minute.
Dial 911 immediately if you experience any sudden loss of function – vision, speech, strength, coordination, sensation, balance, or a new severe headache.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
At the 2015 International Stroke Conference, we heard the results of 4 randomized controlled clinical trials of endovascular therapy for stroke.
Last week we discussed the results of EXTEND-IA (Extending the Time for Thrombolysis in Emergency Neurological Deficits — Intra-Arterial). This week, I present the final published endovascular trial with results presented at the ISC 2015 meeting – The ESCAPE (Endovascular treatment for Small Core and Anterior circulation Proximal occlusion with Emphasis on minimizing CT to recanalization times) trial. The SWIFT-PRIME trial was also presented, but has not been published yet.
- ESCAPE was a randomized controlled trial of intra-arterial therapy versus no intra-arterial therapy for acute ischemic stroke patients.
- If patients were eligible for IV tPA, this was given as standard-of-care, but treatment with IV tPA was not required. 75% of patients received IV tPA before randomization.
- Intra-arterial therapy involved removal of the clot with a stent retriever device. Treatment had to begin within 12 hours from the onset of symptoms.
- To be included, a patient must have a clot detected on a CT scan (CT angiogram) in one of the brain vessels that is a branch of a carotid artery and several other imaging criteria.
- The primary outcome was functional outcome at 90d.
- The treatment with intra-arterial therapy in this trial was very fast; more than half of the patients had recovered blood flow within 1.5 hours after the first CT scan.
- A significantly greater proportion of patients were independent at 90 days in the intra-arterial therapy group than standard-of-care group (0%, vs. 29.3%); death was less frequent in the intra-arterial therapy group.
- The frequency of brain bleeding was similar in the two groups.
- The number of patients who would need to be treated with intra-arterial therapy in order to achieve one additional independent outcome was 4.
In summary, in ESCAPE, the intra-arterial therapy procedure was found to increase the proportion of patients who were independent at 90 days after large artery stroke compared to standard medical therapy. This does NOT mean that intra-arterial therapy is better than IV tPA at treating stroke. This means that AFTER IV tPA, if IV tPA did not open the vessel, there is an additional treatment that could be offered to further improve the chance of a good outcome from stroke. The time from onset of symptoms to treatment with IV tPA was very short. The time from onset of symptoms to the clot-removing treatment was also very short. In clinical practice, similar results would be expected only if the doctors performing the procedures had similar experience and expertise AND the treatments were started as fast as they were in the trial.
Next week, I will discuss the implications of these positive trials on stroke treatment algorithms.
Never forget… During a stroke, every minute counts. Dial 911 immediately if you experience any sudden loss of function – vision, speech, strength, coordination, sensation, balance, or a new severe headache.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
At the 2015 International Stroke Conference , we heard the results of 4 randomized controlled clinical trials of endovascular therapy for stroke.
Last week we discussed the meaning of “randomized controlled trial” and the results of the MR CLEAN – (Multicenter Randomized Clinical trial of Endovascular treatment for Acute ischemic stroke in the Netherlands).
Another randomized controlled trial of endovascular therapy was called EXTEND-IA – (Extending the Time for Thrombolysis in Emergency Neurological Deficits — Intra-Arterial).
- A randomized controlled trial of intra-arterial therapy versus no intra-arterial therapy for acute ischemic stroke.
- All patients first received IV tPA within the first 4.5 hours after the onset of symptoms.
- Patients received either IV tPA alone or intra-arterial therapy with a specific device, called the Solitaire stent retriever.
- To be included, a patient must have a clot detected on a CT scan (CT angiogram) in one of the brain vessels that is a branch of a carotid artery and could not have more than a certain amount of unsalvageable brain tissue.
- The primary outcomes were improvement in blood flow and early neurological improvement. The functional outcome at 90d was also examined.
- This was a small study, because it was stopped early (35 patients in each group). Blood flow was restored in 100% of patients treated with intra-arterial therapy after IV tPA compared to 37% of patients who received IV tPA alone.
- The treatment with intra-arterial therapy in this trial was very fast; half were treated within 3.5 hours from symptom onset.
- More patients who were treated with intra-arterial therapy had early neurological improvement (80% vs 37%); 6x more likely to have early neurological improvement. More patients were independent at 90 days.
- The frequency of brain bleeding was similar in the two groups.
- The number of patients who would need to be treated with intra-arterial therapy after IV tPA in order to achieve one additional independent outcome was 3.2.
In summary, in EXTEND-IA , despite a small number of studied patients, the intra-arterial therapy procedure was found to increase the proportion of patients who were independent at 90 days after large artery stroke compared to standard medical therapy. This does NOT mean that intra-arterial therapy is better than IV tPA at treating stroke. This means that AFTER IV tPA, if IV tPA did not open the vessel, there is an additional treatment that could be offered to further improve the chance of a good outcome from stroke. The time from onset of symptoms to treatment with IV tPA was very short. The time from onset of symptoms to the clot-removing treatment was also very short. In clinical practice, similar results would be expected only if the doctors performing the procedures had similar experience and expertise AND the treatments were started as fast as they were in the trial.
Check back next week for more coverage from the 2015 International Stroke Conference.
Never forget… During a stroke, every minute counts. Dial 911 immediately if you experience any sudden loss of function – vision, speech, strength, coordination, sensation, balance, or a new severe headache.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
At the 2015 International Stroke Conference , we heard the results of 4 randomized controlled clinical trials of endovascular therapy for stroke.
What does “randomized controlled trial” mean? Randomized means that the treating doctors did not choose which treatment the patient received, and that chance alone determined which treatment the patient received. The controlled group received standard medical therapy. A randomized controlled trial should remove the potential for bias in treatment and allow determination of the effect of treatment on outcome.
One example of a randomized controlled trial is known as MR CLEAN – (Multicenter Randomized Clinical trial of Endovascular treatment for Acute ischemic stroke in the Netherlands).
- Initially presented at the 9th World Stroke Congress in October 2014
- A randomized controlled trial of intra-arterial therapy versus no intra-arterial therapy for acute ischemic stroke
- To be included, a patient must have a clot detected on a CT scan (CT angiogram) in one of the brain vessels that is a branch of a carotid artery and must, if randomized to intra-arterial therapy, have the clot removal procedure started within 6 hours of symptom onset
- If patients were eligible for IV tPA, this was given as standard-of-care
- The primary outcome of interest was functional outcome at 90 days
- 500 patients were enrolled; 233 were randomized to intervention and 267 to control treatment
- About 90% of all patients received IV tPA first
- Most of the intra-arterial therapy procedures used the modern retrievable stents
- The study found that patients who had the intra-arterial therapy procedure were 67% more likely to have less disability than patients who did not have the procedure
- The number of patients treated with intra-arterial therapy to get an independent outcome for one more patient than without the treatment was 7
In summary, in MR CLEAN, the intra-arterial therapy procedure was found to increase the proportion of patients who were independent at 90 days after large artery stroke compared to standard medical therapy. This does NOT mean that intra-arterial therapy is better than IV tPA at treating stroke. This means that AFTER IV tPA, if IV tPA did not open the vessel, there is an additional treatment that could be offered to further improve the chance of a good outcome from stroke. The time from onset of symptoms to treatment with IV tPA was very short. The time from onset of symptoms to the clot-removing treatment was also very short. In clinical practice, similar results would be expected only if the doctors performing the procedures had similar experience and expertise AND the treatments were started as fast as they were in the trial.
Check back next week for more coverage from the 2015 International Stroke Conference.
Never forget… During a stroke, every minute counts. Dial 911 immediately if you experience any sudden loss of function – vision, speech, strength, coordination, sensation, balance, or a new severe headache.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
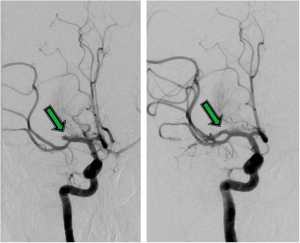
The 2015 International Stroke Conference , which was hosted by Nashville, Tennessee, will forever be remembered by stroke neurologists as the most influential of the 21st century. Why? On Wednesday, February 11th, at the plenary session, conference attendees heard the results of four clinical trials of endovascular therapy for stroke.
Endovascular therapy is treatment inside a vessel. Endo = inside a lumen. Vascular = vessel. During ischemic stroke, blood flow is reduced or stopped to part of the brain, often due to blockage of the vessel by a blood clot. When a patient presents to a hospital within the first few hours after development of stroke symptoms, the patient is rapidly evaluated for treatments which can open blocked vessels. If criteria are met for the intravenous clot-buster, tPA, then tPA should be given as fast as safely feasible, after discussing the risks and benefits. tPA is the standard-of-care for these patients.
If a patient is excluded for treatment with tPA, or does not have an immediate improvement, AND a large artery is blocked by a blood clot, AND treatment could be initiated within 6 hours of onset, endovascular therapy has been considered to be a reasonable treatment. Endovascular therapy involves the patient to be transferred to a special procedure room, called a “cath lab”, where medication for pain and sedation (when needed) is administered, after sterilizing the skin, an artery in the groin or arm is puncture with a needle, and a thin catheter is introduced and advanced until the location of the clot is determined. Using one of several device options, the clot can be treated with direct administration of the clot-buster through a tiny hole at the end of the catheter or be mechanically removed from the artery. The rate of restoring blood flow to the brain with this procedure is about 80%.
While we had evidence that endovascular therapy is highly effective in opening brain arteries, until recently, we did not have evidence that endovascular therapy helped people get better. Next week, I will review the four recent endovascular therapy clinical trials, three of which were presented for the first time this past week. International Stroke Conference 2015 will probably go down in stroke history as the most memorable ISC meeting of the 21st century.
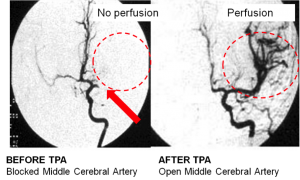
A B
Outcome of endovascular treatment for a patient with an occlusion of a major artery inside the brain. The arrow points to the vessel occlusion before (A) and after (B) treatment.
Never forget… During a stroke, every minute counts. Dial 911 immediately if you experience any sudden loss of function – vision, speech, strength, coordination, sensation, balance, or a new severe headache.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
The International Stroke Conference is a yearly conference provided by the American Heart Association to showcase the latest research ideas and results for an international audience of over 4000 healthcare professionals from over 60 countries. The motto is “connecting the world to stroke science.” We share ideas for process improvement, learn new concepts for prevention and treatment, and learn the results of the latest stroke trials which may impact how we care for patients with stroke.
This year, the International Stroke Conference is in Nashville, Tennessee and starts with “The State of the Science Stroke Nursing Symposium”, “Stroke in the Real World – Working Man Blues: Challenges in Inpatient Stroke Care”, and “Emerging Trends for Stroke Trials: Biomarkers, Adaptive Trial Design, Repair Trials, and New Endpoint” Pre-Conferences on Tuesday, February 10th, followed by 3 days of science providing improved understanding of stroke prevention and treatment.
On prior posts, the focus for acute stroke treatment has been tPA (tissue plasminogen activator – or the “clot buster”) for ischemic stroke and blood pressure control for hemorrhagic stroke. In the next few weeks, the Stroke Tip of the Week will summarize the highlights of the International Stroke Conference.
Without research targeting stroke prevention, acute treatment, and rehabilitation, we cannot advance care. We have a few effective treatments, but they aren’t appropriate or effective for everyone. There are several mechanisms to contribute to stroke research, including donation to the American Heart Association/American Stroke Association.
Never forget… During a stroke, every minute counts. Dial 911 immediately if you experience any sudden loss of function – vision, speech, strength, coordination, sensation, balance, or a new severe headache.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
 Intracranial Aneurysm Screening
Intracranial Aneurysm Screening
Having family members with intracranial aneurysms can increase your risk of having an aneurysm. Familial aneurysms tend to rupture at a smaller size and younger age than sporadic aneurysms.
The risk of aneurysm among family members of patients with aneurysm is also influenced by the risk factors (cigarette smoking, hypertension) that affect aneurysm formation in the general population. If you smoke, it is very important that you quit. If you have high blood pressure, it is very important that your blood pressure is very well controlled.
Screening of unruptured aneurysms remains controversial, but has the potential to prevent life-threatening subarachnoid hemorrhage (SAH), which is bleeding into fluid spaces surrounding the brain.
Two or more affected first-degree relatives — Screening of asymptomatic first-degree relatives (parents, siblings and  children) is generally recommended in families that have two or more individuals with aneurysms. About 8% will have an aneurysm.
children) is generally recommended in families that have two or more individuals with aneurysms. About 8% will have an aneurysm.
It is considered reasonable to screen first-degree relatives every 3 – 5 years with noninvasive brain vessel imaging, such as Magnetic Resonance Angiography (MRA).
One affected first-degree relative — The lifetime risk of SAH for individuals with only one affected first-degree relative is less than 5%.
Guidelines published by the American Stroke Association in 2012 state that while it might be reasonable to offer noninvasive screening, further study is needed to define the risks and benefits of this approach.
It is reasonable to screen first-degree relatives who are >30 years old, are women, and have a history of smoking or hypertension, particularly those who have frequent severe headaches.
Live Prepared, Not Scared
One could argue that being scared of stroke is appropriate. Stroke is the #1 cause of disability in adults. Stroke is the #1 reason for new admission to a nursing home. Stroke is the #5 cause of death in adults. Most of us have had one or more family members or friends who had a disabling stroke. Some of us have had a disabling stroke. Some survivors are more disabled by fear of stroke than they are due to the stroke.
Here are some suggestions for stroke preparedness….
- Know your risk. This means screening for high blood pressure, arrhythmia, diabetes, and high cholesterol. This means owning up to unhealthy habits, such as excessive alcohol use, smoking, and even occasional use of illicit drugs, such as cocaine or methamphetamine.
- Take your prescribed medications. Ensure an adequate supply before travel. Monitor the number of refills each time you fill your prescriptions. Notify your primary care providers of the need for refills as soon as you note you have your last refill filled. Do not wait until you are completely out before reaching out to your health care provider. Keep a list of all prescribed AND over-the-counter medications in your wallet always. Embrace your medications as your protection from stroke.
- In addition to prescribed medications, reduce your risk through lifestyle. Exercise daily, with aerobic activities at for at least 30 minutes at least three times each week. Look for opportunities to burn calories, such as taking the stairs or moving your body while enjoying music or television. Limit sodium in your diet. Limit the amount of food you serve yourself at meals. Make better eating choices, particularly when snacking.
- Know the common symptoms and signs of stroke and heart attacks.
- Know that there are treatments, which can improve outcomes.
- Know that these treatments are time sensitive. The effectiveness of treatment is lessened with each minute that passes.
- Know that calling 911 gives you or your family member/friend the best chance of receiving effective treatment.
- Know that having a list of medications provides information critically needed by professionals while during the fast paced evaluation for receiving the time sensitive treatment for stroke.
- Know that hospital capabilities and efficiencies vary. Some hospitals are better prepared to treat stroke than others, largely due to experience and access to neurological expertise. Research the hospitals in your area, whether in your hometown or vacation spot. Know where you would want to receive emergent stroke treatment.
- If you or a loved one activates 911 services for suspected stroke, please make sure you send an emergency phone # and make sure you know which hospital is the destination so that important and time sensitive exchange of information is handled efficiently.
Live prepared, so you don’t need to be scared. But in the event of sudden loss of function, whether vision, speech, strength, coordination, sensation, or severe headache, call 911 immediately. This is your best chance to get back to normal!
You can search for award-winning hospitals across the country with the American Heart Association map: http://hospitalmaps.heart.org/AHAMAP/map/qimap.jsp.
Obesity
One in 3 Louisiana adults is obese. Louisiana ranks 6th highest in our obesity rate, which has been steadily climbing for the last 20 years.
Obesity contributes to diabetes, hypertension, heart disease, arthritis, and cancer. Many of these conditions contribute to the risk of stroke. You can reduce your chance of having a stroke by reducing your weight. Even losing 5-10% of body weight can positively affect cholesterol levels, blood pressure, blood glucose, sleep apnea, and inflammation, which contributes to development of atherosclerotic plaques. There is also reduced pressure on joints affected by osteoarthritis.
Many people want to lose weight, but have difficulty changing lifestyle, which is necessary to sustaining a plan for healthier choices. The only way to lose weight (without surgery) is to burn more calories than are consumed. Some tips to help you lose weight include:
- Every meal should include something colorful – a fruit or a vegetable.
- Eat the healthier parts of your meal first.
- Get adequate Vitamin C. Vitamin C works against fat storage.
- Learn to recognize the difference between feeling satisfied and feeling full. Stop eating more because it tastes good.
- Drink water throughout the day and at meals. Drink ½ glass of water before your first bite of a meal.
- Limit eating at restaurants. When you do, choose wisely. Try sharing a meal with your partner.
- Replace fattier meats with leaner meats. Chicken and fish are better choices than steak and ground beef.
- Make healthy snacks available and visible.
- If you buy junk food, buy the smallest portions possible.
- If you are going to indulge in dessert, dark chocolate is a good choice due to the antioxidants.
- Reduce the amount of alcohol you consume. Most forms of alcohol add about 100 calories per drink. This can accumulate over time.
- Commercial exercise – While watching television, workout during commercials. There are typically 3 commercials in between program segments. Keep 5 pound weights near you and exercise your biceps, then triceps, and then deltoids during one set of commercials. Try exercises for your hips, thighs, and calves during the next set of commercials. Keeping your muscles tone helps reduce the feeling of work it takes to perform aerobic exercises and improves stamina.
- Alternate toning exercises with aerobic exercises.
- Walk as much as you can. Park further from the entry to your work or shopping center. Walk while you make that phone call in the evening.
- Take the stairs whenever possible. Especially if only 1-2 flights!
- Exercise while brushing your teeth. Try squats and leg lifts in sets of 10.
- 50 stomach crunches before getting out of bed in the morning and before going to bed in the evening.
- Get enough sleep, if possible.

Let’s all try to incorporate some of these tips and reduce our body weight.
Smoking pt. 2
Smoking greatly increases the risk of cancer, heart disease, and stroke. Thousands of Americans who don’t smoke, but are exposed to second hand smoke, die each year from smoking-related illness. Smoking is the most preventable contributor to death in America.
If you are thinking about quitting smoking, please discuss this with your doctor. There are medications and other treatments which can help you in your mission to quit smoking.
Tips recommended by the American Heart Association (AHA) are:
- Set a quit date and sign a No-Smoking contract
- Choose a method for quitting (“cold turkey”, gradual reduction, gradually smoke less of each cigarette).
- Decide if you need medicines to help quit smoking (nicotine replacement and non-nicotine medications).
- Plan for your Quit Day (healthy snacks, rewarding distractions, eliminating cigarettes, lighters, ashtray, and old butts from your environment).
- Stop smoking on your Quit Day (Yay!, Congratulate yourself on your new beginning. Your breathing will improve within days).
Please consider visiting the American Heart Association website for access to frequently asked questions about quitting smoking, a calculator to determine the financial cost of smoking, a smokers confidence assessment, tips for smoking quitters, and educational brochures. The links to the following websites are also available here.
- American Cancer Society
Toll-free hotline: 1-800-ACS-2345 (1-800-227-2345)
www.cancer.org* - American Lung Association
Toll-free hotline: 1-800-LUNGUSA (1-800-586-4872)
www.lungusa.org* - MedLine Plus – Local Smoking Cessation Resources (from the National Library of Medicine and the National Institutes of Health)
http://www.nlm.nih.gov/medlineplus/golocal/topicmap_1359.html* - National Cancer Institute
Toll-free hotline: 1-877-44U-QUIT (1-877-448-7848)
www.smokefree.gov* - National Institutes of Health – Clinical Trials on Smoking Cessation
http://clinicaltrials.gov/search/open/condition=%22Smoking+Cessation%22* - National Network of Tobacco Cessation Quitlines
Toll free hotline: 1-800-QUITNOW (1-800-784-8669)
TTY: 1-800-332-8615
www.naquitline.org*
Let’s all make 2015 a healthier year! You have this within your control. You can do this 
Smoking

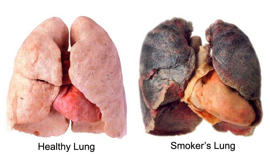
Smoking increases the risk of many serious health conditions, including stroke and heart disease. The risk of stroke with smoking one pack per day is 6x that of a nonsmoker. Even if you smoke less than one pack per day, your risk of stroke is about 3x that of a nonsmoker.
The brain needs a healthy heart to provide blood flow. The brain needs healthy arteries to deliver the blood flow. Smoking injures your arteries by:
1) exposing the lining of the arteries to damaging chemicals,
2) shifting the ratio of good “protective” cholesterol and bad “damaging” cholesterol,
3) increasing the stickiness of blood and the number of platelets (contribute to clots),
4) accelerating the development of atherosclerosis, and
5) making clots more likely to form on the surface of diseased vessels.
Smoking, in combination with high blood pressure, increases the risk of subarachnoid hemorrhage, a devastating type of stroke caused by a ruptured aneurysm, or weakened and ballooning artery in the brain.
The good news is that the percentage of US citizens who smoke has gone down over time, but about one in five people still smoke. More good news is that the reduction in the risk of stroke occurs within 5 years after quitting smoking.
If you are thinking about quitting smoking, please discuss this with your doctor. There are medications and other treatments that can help you in your mission to quit smoking.
Let’s all make 2015 a healthier year!
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
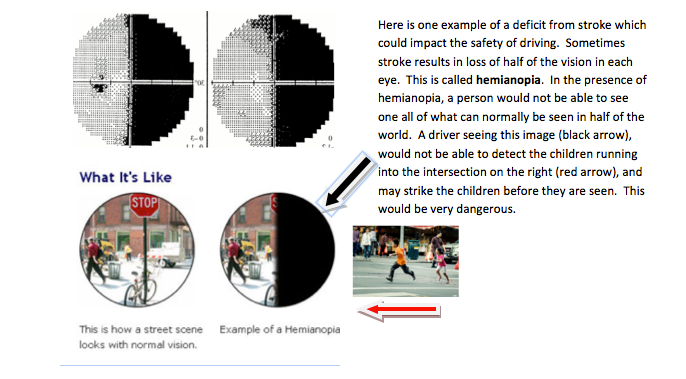
Operating a Vehicle after Stroke
Neurologists want their patients to be as independent as possible and to recover pre-stroke activities, including driving, provided it is safe to do so. However, stroke can affect one or more of several brain functions crucial to safely operating a vehicle. These include:
- Vision
- Control of eye movements
- Attention
- Reading of street signs
- Ability to handle a steering wheel
- Ability to handle the foot pedals
- Response time
In one study of over 1,700 stroke patients, about half recovered driving capacity between 2 and 9 months after stroke. Success rates between 24% and 88% have been reported. Success may be predicted by 3 office-based tests called Road Sign Recognition, Compass, and Trail Making Test part B.
Devos H, Akinwuntan AE, Nieuwboer A, Truijen S, Tant M, De Weerdt W. Screening for fitness to drive after stroke: a systematic review and meta-analysis. Neurology 2011;76:747–756.
Sometimes, it is obvious to you or your doctor that you cannot safely drive. Sometimes, your doctor will be uncertain. You may require referral for formal driving assessment and therapy. Professionals can evaluate your vision, functional ability, response/reaction time, thinking, and problem solving abilities and performance behind the wheel of a car. Fees apply and are not covered by insurance, unfortunately.
Please ask your doctor and/or occupational therapist about driving before doing so on your own. Please do not jeopardize your recovery or the health of others by driving before you are ready. Your State Department of Motor Vehicles may be a valuable resource.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Depression after Stroke
Depression after stroke is common, affecting about 1 in 5 people. Stroke potentially changes chemicals in the brain, promoting depression. Depression is highly associated with more severe physical impairment and less improvement after stroke, compared with non-depressed patients with stroke, and can become a barrier to improving with therapies.
Common symptoms of depression include:
- Feeling sad, hopeless or “empty”
- Feeling worthless and helpless
- Feeling irritated, anxious, angry
- Slowed processing, impaired concentration, poor memory
- Unexplained aches and pains
- Poor energy
- Loss of interest in pleasurable activities
- Sleeping too much or too little with trouble getting or falling asleep
- Eating too much or not enough
- Suicidal thoughts
Feelings of grief and loss are normal after a stroke. Many of the listed symptoms are common during the adjustment phase after stroke. If symptoms accumulate or worsen over time, you need medical attention.
Depression is largely treatable with medications and therapy. Treatment of depression is associated with lower death rates after stroke. Antidepressants given to stroke patients, even those without depression, may lead to greater improvement in cognition, communication, and motor function than placebo during rehabilitation. Other ways to prevent or treat depression include:
- Learning more about stroke
- Document progress in rehab
- Talk about your feelings with family and friends
- Stay as active as possible with prior hobbies
- Abstain from alcohol.
If you or a loved one have symptoms of depression, please communicate this with your doctor. If there are thoughts of suicide, immediate attention is needed.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Physical Rehabilitation & Recovery – The 9th P of Stroke
Last week, we reviewed the 8th P of stroke – Penumbra. This week, we will review the 9th P of stroke – Physical Rehabilitation & Recovery.
Stroke is the leading cause of adult disability. Rehab after stroke is crucial to reduce the longterm disability associated with stroke. Therapeutic interventions, including physical therapy (PT), occupational therapy (OT), and speech/ language pathology (SLP) can promote functional improvement.
Physical therapists evaluate motor and sensory disabilities following a stroke and develop a plan of care to promote return of function. The discipline focuses on walking, range of motion, balance, and alleviating joint pains, falls, prevention and management of pressure sores, foot drop, and paralysis. Repetitions of these movements help the brain relearn how to control muscles and completing a therapy plan of care can enhance recovery of function.
Occupational therapy encourages the development of lost skills to enhance performance of activities of daily living (ADLs). Through training that is focused on deficits in relation to fine motor movements, vision, attention, and neglect, OT can reduce dependence on caregivers and the need for alternative living situations.
Speech and language pathologists identify deficits and methods for improvement with regards to language, cognition, impulsivity, inattentiveness, or neglect to promote improvement in production and quality of speech, expressive and receptive language, swallowing abilities, and cognitive aspects. Therapies are initiated during the acute hospitalization once the patient is able to actively participate.
Early mobilization was studied in the A Very Early Rehabilitation Trial for stroke (AVERT) and was found to be safe at 24 hours post acute stroke (Bernhardt, Dewey, Thrift, Collier & Donnan, 2008). Increasing activity can decrease risk of complications such as venous thromboembolism, pneumonias, and skin breakdown and can promote a more rapid recovery. Therapy following the acute hospital stay is vital in stroke recovery and a multidisciplinary approach should be used in determining which setting is appropriate for the patient’s next level of care based on their individual medical, rehabilitation, and personal needs at the time of discharge. Options include outpatient therapies in outpatient centers or through home health services, skilled nursing facilities and nursing homes, or in an inpatient setting including long term acute care (LTAC) hospitals or inpatient rehabilitation centers (IRF). Inpatient rehabilitation is the most intense level of therapy with patients receiving at least three hours of individualized therapies daily along with care from a physician with specialty training in rehabilitation medicine, rehabilitation nursing, recreational therapy, case management, and preparation for discharge, including family training and education, to reduce burden of care upon discharge. Assistive devices for mobility such as wheelchairs, walkers, or canes, and equipment used for activities of daily living, such as tub benches, shower chairs, and toileting devices may assist in achieving increased independence. Customized splints may be recommended for positioning of limbs affected by paresis or paralysis.
With up to 2 million brain cells dying every minute during a stroke, please remember to CALL 911 IMMEDIATELY FOR ANY SUDDEN LOSS OF FUNCTION – vision, speech, strength, coordination, sensation, or severe headache. This is your best chance to save PENUMBRA and get back to your life!
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Penumbra – The 8th P of Stroke
Last week, we reviewed the 7th P of stroke – Parenchyma. This week, we will review the 8th P of stroke – Penumbra.
Penumbra is the part of the brain tissue that can be recovered if blood flow is restored during an ischemic stroke. Within the penumbra, blood flow is low enough that the tissue cannot serve its particular function (such as speech production), but is still capable of performing the steps required to keep the brain cells alive. The penumbra is the target when the clotbuster medication, tPA, or other procedures to open blocked arteries are attempted.
The major determinants of whether a brain cell dies include 1) how low the blood flow is and 2) how long the blood flow is low. If blood flow is severely reduced, brain cells die rapidly, penumbra will be lost, and the stroke will complete much faster than if there is a mild reduction in flow. Once the tissue is infarcted, the cells cannot survive, even if the blood flow is restored. The penumbra is dynamic in that about 2 million brain cells die every minute during a stroke.
The presence or absence of penumbra can be determined by advance brain imaging.
With up to 2 million brain cells dying every minute during a stroke, please remember to CALL 911 IMMEDIATELY FOR ANY SUDDEN LOSS OF FUNCTION – vision, speech, strength, coordination, sensation, or severe headache. This is your best chance to save PENUMBRA and get back to your life!
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Parenchyma – The 7th P of Stroke
Last week, we reviewed the 6th P of stroke – Perfusion. This week, we will review the 7th P of stroke – Parenchyma.
Parenchyma is the brain tissue.
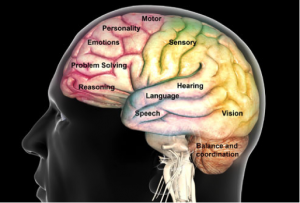
Every part of the brain has its own special function. Even the two sides of the brain are responsible for different functions. Damage to the brain, from whatever cause, leads to loss or abnormal function specific to the location of
the damage. Brain imaging is most commonly achieved with CT (computerized tomography or “cat scan”) or MRI (magnetic resonance imaging). In the first few hours after onset of stroke symptoms, the most important brain imaging test is the CT scan. This will distinguish between the two types of stroke – ischemic and hemorrhagic.
 In the first few hours of stroke, there may be no changes on the CT scan of the brain. With a hemorrhagic stroke, you can see blood, because it appears white relative to other parts of the brain. It is critically important to rule out any blood on CT scan of the brain before being treated with the clotbuster for an ischemic stroke. The brain is best imaged by MRI, but not all patients can have an MRI (pacemaker, for example) or tolerate it (claustrophobia).
In the first few hours of stroke, there may be no changes on the CT scan of the brain. With a hemorrhagic stroke, you can see blood, because it appears white relative to other parts of the brain. It is critically important to rule out any blood on CT scan of the brain before being treated with the clotbuster for an ischemic stroke. The brain is best imaged by MRI, but not all patients can have an MRI (pacemaker, for example) or tolerate it (claustrophobia).
Parenchymal (brain)imaging is part of the standard evaluation for many conditions – stroke, traumatic brain injury, dementia, headache, multiple sclerosis, brain tumors and many other complaints and disorders.
A) Ischemic stroke on MI image B) Hemorrhagic stroke on CT image
REMEMBER – CALL 911 IMMEDIATELY FOR ANY SUDDEN LOSS OF FUNCTION – vision, speech, strength, coordination, sensation, or severe headache. This is your best chance to get back to normal.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Perfusion – The 6th P of Stroke
Last week, we reviewed the 5th P of stroke – Plumbing. This week, we will review the 6th P of stroke – Perfusion
Perfusion is the movement of a liquid (perfusate/blood) through a tissue (parenchyma/brain).
Factors impacting perfusion include the output from the heart, blood pressure, blood viscosity, pipe narrowing or occlusion (all described in previous tips of the week), pressure inside of the brain tissue and draining from veins. During an ischemic stroke, placing the head flat increases perfusion of the brain. In contrast, raising the head can decrease perfusion and pressure on a broken blood vessel in the setting of a hemorrhagic stroke.
The two determinants of whether a brain cell dies during a stroke are the depth of low blood flow and the duration of low blood flow. If the flow is only mildly reduced, brain cells can live longer than if the flow is severely reduced. Advanced brain imaging with CT or MRI can provide information about perfusion. Where there is no perfusion, brain cells die rapidly. Where there is slow perfusion, brain cells may be saved if blood flow is improved. The goal of treating ischemic stroke is to establish reperfusion before brain cells are dead. The standard treatment to achieve reperfusion is tPA, the clot buster that can be administered in the first few hours after stroke onset, provided there are no contraindications (patient characteristics which increase the risk of the medication or reduce the benefit).
REMEMBER – CALL 911 IMMEDIATELY FOR ANY SUDDEN LOSS OF FUNCTION – vision, speech, strength, coordination, sensation, or severe headache. This is your best chance to get back to normal.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Plumbing – The 5th P of Stroke
Last week, we reviewed the 4th P of stroke – the Pipes. This week, we will review the 5th P of stroke – Plumbing
“PLUMBING” – describes the communication, or connection, between arteries in the brain. Not everyone has the same configuration of pipes. If there is good plumbing, the damage from loss of a single vessel may be minimized. Good plumbing provides a natural bypass when one pipe becomes obstructed. In this situation, occlusion of a pipe, even a carotid artery, can be clinically silent and without brain injury. “Communicating vessels” can connect arteries from one side of the brain to the other side or provide opportunities for flow from the arteries in the front of the brain to those in the back of the brain, including the brainstem.
Poor plumbing makes areas of the brain dependent on a single pipe for blood flow to a discrete region. In this situation, occlusion of a pipe can cause total territorial damage and can be devastating. In some situations, improved plumbing is created through surgical intervention by connecting a pipe from outside of the skull to one inside of the skull to provide a bypass and supply blood to the brain.
It is very important to protect your existing plumbing by protecting your pipes. Keeping blood pressure, glucose, and cholesterol under control, and abstaining from smoking are very important ways to keep your pipes and, therefore, plumbing healthy.
REMEMBER – CALL 911 IMMEDIATELY FOR ANY SUDDEN LOSS OF FUNCTION – vision, speech, strength, coordination, sensation, or severe headache. This is your best chance to get back to normal.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Pipes – The 4th P of Stroke
Last week, we reviewed the 3rd P of stroke – the Perfusate. This week, we will review the 4th P of stroke – Pipes
The pipes are the arteries, or the tubes through which the perfusate (blood) travels from the pump (heart) to the brain. These pipes have multiple branches, similar to an oak tree.
 Much of stroke prevention is focused on protecting the pipes, including blood pressure, glucose, and cholesterol control and avoidance of smoking tobacco products. When the pipes become damaged, they start collecting fat and calcium with resulting atherosclerosis. As atherosclerosis develops, the opening (or lumen) of the pipe becomes narrowed and flow can be compromised. When a pipe becomes completely blocked, like when a clot travels from the heart and lodges inside of a brain pipe (artery), the brain tissue that depends on that pipe for blood delivery stops functioning, symptoms develop, and the brain tissue dies unless the pipe opens quickly. There are many options for imaging the pipes, including CT and MRI scans, invasive angiograms, and ultrasound. If a pipe is significantly narrow and causes symptoms, your doctor may discuss opening the pipe with surgery or a stent. It is not known if a narrow pipe without symptoms should be opened. Ongoing clinical trials will address this situation for carotid artery narrowing in the neck.
Much of stroke prevention is focused on protecting the pipes, including blood pressure, glucose, and cholesterol control and avoidance of smoking tobacco products. When the pipes become damaged, they start collecting fat and calcium with resulting atherosclerosis. As atherosclerosis develops, the opening (or lumen) of the pipe becomes narrowed and flow can be compromised. When a pipe becomes completely blocked, like when a clot travels from the heart and lodges inside of a brain pipe (artery), the brain tissue that depends on that pipe for blood delivery stops functioning, symptoms develop, and the brain tissue dies unless the pipe opens quickly. There are many options for imaging the pipes, including CT and MRI scans, invasive angiograms, and ultrasound. If a pipe is significantly narrow and causes symptoms, your doctor may discuss opening the pipe with surgery or a stent. It is not known if a narrow pipe without symptoms should be opened. Ongoing clinical trials will address this situation for carotid artery narrowing in the neck.
There are many other causes of damage to pipes, including tears resulting from trauma and inflammation or spasm after exposure to amphetamines, like cocaine. These causes are far less common than atherosclerotic disease.
REMEMBER – CALL 911 IMMEDIATELY FOR ANY SUDDEN LOSS OF FUNCTION – vision, speech, strength, coordination, sensation, or severe headache. This is your best chance to get back to normal.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Perfusate – The 3rd P of Stroke
Last week, we reviewed the 2nd P of stroke – the Pressure. This week, we will review the 3rd P of stroke – Perfusate.
Perfusate is the liquid (blood) that moves through a solid organ, like the brain. Blood volume, content, thickness, and clotting are issues of perfusate.
The perfusate must have a sufficient volume to generate blood pressure within the arteries. If the volume of blood is low, the pressure will be lower (see Tip of the Week October 20, 2014), and evaluation for the cause of the low blood volume is necessary.
The perfusate must carry sufficient content of oxygen and glucose. Oxygen and glucose are necessary for brain cells to function properly – in terms of the steps needed for the cells to stay alive and keep doing the special function of the cells in a particular part of the brain (for example, speech, movement, or vision).
The perfusate should not be too viscous (thick). Increased viscosity of blood occurs in conditions where the concentrations of cells or large proteins are greater than normal or where the shapes of cells are not normal (sickle cell anemia). Examples include: too many red blood cells (polycythemia vera), too many platelets (thrombocytosis), too many white cells or immune cells (leukemia). Increase in viscosity can increase the risk for strokes due to sludging in the microcirculation.
The perfusate should not be prone to clotting. Some patients have gene mutations or abnormal clotting factors. Laboratory analysis for known arterial or venous clotting abnormalities may be warranted when a young person (<50yo) has a stroke or other clotting event (such as blood clot in the vein of a limb or a heart attack).
REMEMBER – CALL 911 IMMEDIATELY FOR ANY SUDDEN LOSS OF FUNCTION – vision, speech, strength, coordination, sensation, or severe headache. This is your best chance to get back to normal.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Pressure – The 2nd P of Stroke
Last week, we reviewed the 1st P of stroke – the Pump. This week, we will review the 2nd P of stroke – Pressure
 If you think back to our sketch from last week’s Tip of the Week, the pump will eject blood from the heart and up through to the aorta and all of the arteries that travel throughout the body, including the brain. Blood pressure is the driving force for delivering that blood to where it needs to go.
If you think back to our sketch from last week’s Tip of the Week, the pump will eject blood from the heart and up through to the aorta and all of the arteries that travel throughout the body, including the brain. Blood pressure is the driving force for delivering that blood to where it needs to go.
The basic concept is – too little pressure -> brain and other organs stop functioning properly. If the pressure is low for a short amount of time, recovery is expected. If blood pressure and flow are too low to meet the needs of the brain and other organs for too long, damage may be permanent. When this happens to the brain, it is a stroke.
If the pressure in the brain is too low for the “brain sprinklers” to get blood to all parts of the brain, the amount of oxygen and glucose supplied to the brain will be lower than the demands of the brain. When the pressure, and, therefore, flow is reduced through a specific brain artery which supplies a specific part of the brain which has a specific function, that function will be lost, and the person experiences symptoms and signs of STROKE. The brain can only tolerate low pressure for a short time before brain cells start to die.
When there is too much force, however, the blood vessels inside of the brain can break under the pressure, resulting in bleeding into the brain. High blood pressure is the #1 cause of brain hemorrhage, the second most common form of stroke. Therefore, most brain hemorrhages are preventable by keeping blood pressure normal. Having normal blood pressure depends on having it measured and treated, if recordings of over 140/90 are measured on more than one occasion. The September 8, 2014 Tip of the Week provides a list of behavioral changes that can reduce blood pressure.
REMEMBER – CALL 911 IMMEDIATELY FOR ANY SUDDEN LOSS OF FUNCTION – vision, speech, strength, coordination, sensation, or severe headache. This is your best chance to get back to normal.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
The Pump – The 1st P of Stroke
In the last 3 weeks, I introduced the 10th P of Stroke – Prevention. Now I will start from the beginning. The 1st P of stroke is the Pump.
 The heart acts as the “pump” for moving blood throughout the body. The pump helps to deliver oxygen and glucose (a type of sugar in the blood) to the brain, which allows us to have adequate energy metabolism and function properly.
The heart acts as the “pump” for moving blood throughout the body. The pump helps to deliver oxygen and glucose (a type of sugar in the blood) to the brain, which allows us to have adequate energy metabolism and function properly.
Essential to the cardiac workup is detection of clots (known as thrombi). Thrombi formed in the heart can travel (embolize) through the arteries (or pipes) that bring blood to the brain, resulting in blockage of blood flow to part of the brain, resulting in stroke. This type of stroke, known as cardioembolic stroke, makes up approximately 25% of all ischemic strokes. Several defects in cardiac structure or function increase the risk for formation of clots, most of which share the underlying physiology of stagnation of blood flow (meaning slowing of flow). Common examples of this include, but are not limited to, atrial fibrillation (see previous tip of the week) and severely reduced pump strength. Emboli can also originate on the heart valves and can be either non-infectious or infectious in nature.
A patent foramen ovale (PFO) is a small tunnel connecting the top chamber of one side of the heart with the top chamber of the other side of the heart. This illustrates the concept of paradoxical emboli as a cardioembolic stroke risk factor, meaning that blood clots formed within veins can travel directly to the arterial system without getting stuck in the blood flow of the lungs. If a PFO is found within the heart of a patient with stroke, a search for DVT (clot in the veins of the arms & legs) may be completed to find the source.
Electrocardiography (EKG) can identify abnormal rhythms (such as atrial fibrillation) or evidence of significant chamber enlargement. Traditionally, echocardiography (ultrasound of the heart) is performed with a TTE (transthoracic echocardiography with imaging of the heart across the chest wall), which allows for visualization of heart function, the presence of chronic hypertensive heart disease (see prior tip on hypertension), and valvular dysfunction or malformation, such as aortic stenosis. Evidence of other entities mentioned above such as clots or valve abnormalities may also be visible if large enough.
These entities may only be detected by transesophageal (TEE) viewing, which requires swallowing an ultrasound probe and imaging the heart from behind the heart with the probe in the esophagus. TEE allows for a higher resolution and is better to detect thrombi, evidence of blood stagnation, and PFO. A “bubble study” may be performed as a component of the echocardiogram, which includes injecting agitated saline or contrast through the venous circulation to detect visualization of the saline bubbles passing through to the left side of the heart in the presence of an intracardiac shunt.
Keeping your heart healthy through diet and exercise, avoiding toxins, such as overuse of alcohol or stimulants, and keeping your blood pressure under control (<140/90) can prevent the changes in rhythm and function of the heart contributing to the risk of stroke.
REMEMBER – CALL 911 IMMEDIATELY FOR ANY SUDDEN LOSS OF FUNCTION – vision, speech, strength, coordination, sensation, or severe headache. This is your best chance to get back to normal.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Prevention (Part 3) – The 10th P of Stroke
Two weeks ago, I introduced the 10th P of Stroke = Prevention
Most strokes are preventable. A risk factor is a condition that, compared to persons without the condition, increases the chance of an outcome, like stroke.
Obstructive sleep apnea (OSA) is a risk factor for stroke and up to 1 in every 15 people have this condition. OSA is more common in men, because the amount of tissue in the neck is generally larger for men. However, if OSA is present, the stroke risk is similar in men and women.
OSA occurs when the tissues and/or tongue relax during sleep and put pressure on the airway, obstructing the normal movement of air. Oxygen goes down and carbon dioxide goes up. These changes in gases are detrimental to the heart and blood vessels, including those of the brain. Over time, blood pressure becomes more difficult to control, abnormal heart rhythms can occur, and stroke may occur. Chronic OSA can also lead to memory impairment (dementia) due to low oxygen causing brain cells to die prematurely. The chronic elevation in blood pressure can provoke heart failure, which further increases the risk of stroke.
Symptoms of OSA include: snoring, daytime sleepiness, headaches present upon awakening, dry mouth upon awakening, trouble concentrating, and poor sleep quality. A bed partner may witness pauses in breathing.
OSA is diagnosed with a polysomnogram, or “sleep study,” during which breathing and oxygen are monitored. If OSA is diagnosed, the standard treatment is CPAP or continuous positive airway pressure. This extra pressure helps to keep the airway open and improve the exchange of gases. The pressure is administered by a machine through tubing and a facial mask. Some people have trouble tolerating the mask, but many note substantially improved sleep!
Other treatments to reduce the impact of OSA on the body include:
- Weight loss to reduce the amount of tissue that relaxes during sleep.
- Nasal decongestants to reduce the contribution of snoring by edematous nasal passages.
- Sleeping in the side position, rather than the back.
- Surgery to reduce the amount of tissue that relaxes during sleep.
- Oral appliances to hold the tongue and jaw in a position least likely to result in pressure on the airway.
Live your life PREPARED – not SCARED!
REMEMBER – CALL 911 IMMEDIATELY FOR ANY SUDDEN LOSS OF FUNCTION – vision, speech, strength, coordination, sensation, or severe headache. This is your best chance to get back to normal.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Prevention (Part 2) – The 10th P of Stroke
Last week, I introduced the 10th P of Stroke: Prevention
Most strokes are preventable. A risk factor is a condition that, compared to persons without the condition, increases the chance of an outcome, like stroke. Research shows women’s stroke risk is influenced by hormones, reproductive health, pregnancy, childbirth, and other gender-related factors.
The American Heart Association/American Stroke Association Guidelines for the Prevention of Stroke in Women was published in 2014.
Highlights include:
- Women who have migraine headaches with aura should stay away from smoking to avoid higher stroke risks.
- Women should be screened for high blood pressure before taking birth control pills because the combination raises stroke risks.
- Pregnant women with moderately high blood pressure (150-159 mmHg/100-109 mmHg) may be considered for blood pressure medication, whereas expectant mothers with severe high blood pressure (160/110 mmHg or above) should be treated.
- Women with a history of high blood pressure before pregnancy should be considered for low-dose aspirin and/or calcium supplement therapy to lower preeclampsia risks.
- Women with preeclampsia have twice the risk of stroke and a four-fold risk of high blood pressure later in life. Therefore, preeclampsia should be recognized as a risk factor well after pregnancy, and other risk factors such as smoking, high cholesterol, and obesity in these women should be treated early. (Preeclampsia is a blood pressure disorder during pregnancy that causes major complications, including stroke during or after delivery, premature birth, and risk of stroke well after child-bearing.)
- Women over age 75 should be screened for atrial fibrillation risks as it is linked to higher stroke risk.
Live your life PREPARED – not SCARED!
REMEMBER – CALL 911 IMMEDIATELY FOR ANY SUDDEN LOSS OF FUNCTION – vision, speech, strength, coordination, sensation, or severe headache. This is your best chance to get back to normal.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Prevention – The 10th P of Stroke
Over the next couple of months, I will introduce the 10 P’s of Stroke. Over the next 3 weeks, I will cover the 10th P – Prevention.
Most strokes are preventable. A risk factor is a condition that, compared to persons without the condition, increases the chance of an outcome, like stroke. There are many known risk factors for having a stroke. These are the estimated impacts of some common risk factors:
In many cases, medications must be taken to reduce the severity of these risk factors. Embrace those medications as protection for your brain. You can reduce the need for medications by modifying your behavior and diet. Significant reduction in blood pressure can be achieved, for example, through limiting salt and alcohol in the diet, increasing physical activity, reducing body weight, and treating obstructive sleep apnea.
Please speak with your primary care doctor. You need to know:
- Which risk factors you have.
- Whether your risk factors are under control.
- How you can improve the control of your risk factors.
Live your life PREPARED – not SCARED!
REMEMBER – CALL 911 IMMEDIATELY FOR ANY SUDDEN LOSS OF FUNCTION – vision, speech, strength, coordination, sensation, or severe headache. This is your best chance to get back to normal.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
September is Atrial Fibrillation Awareness Month

The atrium is the upper part of the heart. Fibrillation means fast incoordinated contraction of muscle. When the muscle of the atrium fibrillates, we call this atrial fibrillation. Atrial fibrillation, or Afib, is a consequence of chronic high blood pressure, other forms of heart disease, thyroid gland dysfunction, or even exposure to stimulants, such as caffeine or nicotine, and alcohol.
Because not every contraction of the atrium leads to a contraction of the ventricle, the heartbeat is irregular and the amount of blood inside the ventricle is also irregular. Some people with atrial fibrillation have no symptoms until stroke occurs but may notice an irregular pulse. Others experience a rapid and irregular heartbeat that may be perceived as pounding or rumbling, or shortness of breath, fatigue, chest pain, dizziness, or may lose consciousness.
When the atrium fibrillates, the blood is not forcefully ejected into the ventricle, but recirculates and may form into a blood clot. If the blood clot makes it out of the heart, it can travel, or embolize, to other parts of the body. When the clot lodges inside of an artery in the brain, it causes stroke. Atrial fibrillation is a common cause of stroke, especially with advancing age. Stroke due to atrial fibrillation is largely preventable with medications that prevent the recirculating blood from forming a clot.
Check your PulseSM at least once each month and determine if the beat is regular or if the time between beats is irregular. Feel your pulse at the wrist for a full minute. If you think the pulse is irregular, consult with your doctor.
Call 911 for ANY sudden loss of function, whether vision, speech, strength, coordination, sensation, or ability to walk OR for a sudden severe and unexplainable headache.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Elevated Blood Pressure – Hypertension
Hypertension is defined as blood pressure more than 140/90. The top number is the systolic blood pressure, which is the pressure in the arteries at the time the heart ejects blood out after collecting in the chamber called the ventricle. The bottom number is the diastolic blood pressure, which is the pressure in the arteries at the time the heart is relaxing and filling the ventricle with blood. Both numbers are important. High pressures put stress on your heart and arteries throughout the body, making the arteries fragile and triggering the formation of atherosclerosis.
Hypertension is the most important controllable risk factor for stroke. If all blood pressure were controlled, close to half of all strokes would be prevented. Hypertension is a silent killer, because it can be present for years, causing damage to your organs, including heart, kidneys, eyes, and brain before symptoms develop. If identified and treated before these organs fail, permanent damage can be prevented. Even if you think you are perfectly healthy and have never been told you have high blood pressure, your blood pressure should be screened at a minimum every 2 years, but screening more frequently is harmless.
If you have hypertension, your primary care provider will help decide if medication is needed to control your blood pressure, and, if so, which medication is most appropriate for you. There are other behavioral changes you can make to help control blood pressure, including low dietary sodium intake, increased physical activity, weight loss, reduction of alcohol intake, treatment of obstructive sleep apnea, and stress relief.
Call 911 for ANY sudden loss of function, whether vision, speech, strength, coordination, sensation, or ability to walk OR for a sudden severe and unexplainable headache.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director
Vision Loss
One of the common symptoms of stroke is vision loss. Vision loss is generally sudden in onset. Common patterns suggestive of stroke include:
- Sudden monocular (one eye) painless visual loss. This often represents loss of blood flow to the retina. Did you know that the retina is part of the brain? Loss of vision in one eye due to loss of blood flow is actually a stroke. Pain with visual loss is not usually related to stroke, but may represent another type of emergency, where treatment must be given quickly to restore vision.
- Sudden double vision. This means that two objects are seen, when it is known that there is only one object. Double vision (also called diplopia) may be side by side, images on top and bottom, or even diagonal. This is often related to stroke in the brainstem, where the nerves that control the eye muscles come from.
- Sudden restricted vision on one side, left or right. This may be perceived as trouble seeing in one eye. To tell the difference, one eye can be covered and vision rechecked. If one side is still not seen, even though one eye is covered (or closed), this is very likely to be due to a stroke. If a person has to turn their head in order to see everything in the periphery he or she can normally see, this could be due to a stroke.
Any sudden loss of vision should be presumed to be due to stroke until proven otherwise. When both eyes are looking to one side and there is loss of the ability to fully move the eyes to the opposite side, this too may indicate stroke.
Call 911 for ANY sudden loss of function, whether vision, speech, strength, coordination, sensation, or ability to walk OR for a sudden severe and unexplainable headache.
Until next week,
Sheryl Martin-Schild, MD, PhD, FANA, FAHA
LERN Stroke Medical Director