U.S.TRAUMA SYSTEM HISTORY
The beginnings of modern trauma systems in the United States can be traced to federal legislation, specifically the Highway Safety Act of 1966 and the Emergency Medical Services Systems Act of 1973. These acts represent our initial efforts to apply the emergency medical and trauma care lessons learned by physicians serving in the military during the wars in Korea and Vietnam. The acts led to education and training programs for emergency medical technicians (EMTs) and initial model development of regional trauma and emergency medical services.
These early efforts were a huge step forward, but the model of trauma care developed was limited, emphasizing hospital-based acute care. The next major step forward in trauma care policy was the development of Model Trauma Care Systems Plan in 1992 by the Health Resources and Services Administration (HRSA) – a new model that called for an inclusive trauma care system. This new inclusive trauma system model included not only trauma centers, but all health care facilities according to availability of trauma resources.
In 2002, HRSA conducted the National Assessment of State Trauma System Development, Emergency Medical Services Resources, and Disaster Readiness for Mass Casualty Events. This study demonstrated much progress but also revealed that few states could boast of trauma systems that included all the components of HRSA’s inclusive trauma system model. Not surprisingly, this assessment also demonstrated that states with the most comprehensively developed trauma systems were more ready to medically handle disasters of all types.
In 2006, HRSA updated its trauma system model with the publication of Model Trauma Systems Planning and Evaluation. This update to the model utilizes a public health framework that views traumatic injury as a disease that can be prevented or managed in a way that reduces severity and improves ultimate outcome.
Today, the nationally recognized resource for development of statewide trauma systems is Resources for Optimal Care of the Injured Patient by the American College of Surgeons (ACS) Committee on Trauma. This guidebook provides the detailed descriptions of the organization, staffing, facilities, and equipment needed to provide state-of-the-art treatment for the injured patient at every phase of trauma system participation. LERN is using this guidebook to develop an inclusive statewide trauma system in Louisiana.
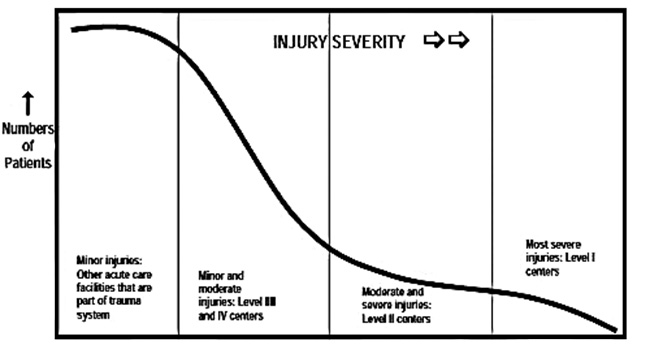
The inclusive trauma system model recognizes the full continuum of injury severity and utilizes all acute care facilities to get the injured patient to the Right Place at the Right Time to receive the Right Care.
Inclusive Trauma System Model
Resources for the Optimal Care of the Injured Patient, 2014
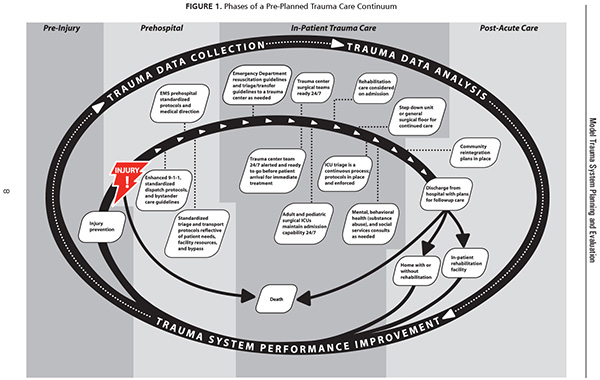
A statewide trauma care system has many components – requiring a multidisciplinary team approach that allows all involved health care providers to function in pre-planned concert. Emergency care providers match patients, through protocols and medical supervision, with the medical facility equipped with the resources to best meet the patient’s needs – sometimes bypassing the closest medical facility.
See figure below, which illustrates the pre-planned, seamless flow of trauma care delivery for those experiencing severe injury. (Click image to see full-sized PDF)